If you do not see your coverage amounts and co-pays on your health insurance card, call your insurance company . Ask what your coverage amounts and co-pays are, and find out if you have different amounts and co-pays for different doctors and other health care providers. The HCBS waiver is designed to provide services to supplement informal supports for... This service helps members manage their physical and behavioral health care needs through education, support, and advocacy.
Children's Mental Health Wraparound Program Children's Mental Health Wraparound Program Indiana Medicaid offers coverage for the Child Mental Health Wraparound home and community-based services . The CMHW HCBS program provides services to youth, ages 6-17, who have a diagnosis of a serious emotional disturbance . Electronic Visit Verification Electronic Visit Verification On or before January 1, 2020, some Indiana Medicaid providers will begin to use a system called Electronic Visit Verification. The pilot part of this new process will begin July 1, 2019, so you may see your provider use the new system soon. Provider Directory Provider Directory Start here to find a Medicaid provider near you. Managed Care Health Plans Managed Care Health Plans Depending on your eligibility, you may be enrolled with a health plan to help coordinate and manage your healthcare.
Find out more about health plan options and how to contact them. Authorized Representative Form Authorized Representative Form In certain cases, you may need to have an authorized representative communicate with your caseworker or Medicaid staff. In order for the State to discuss your case or history with your representative, you will need to give written permission. Member Appeals Member Appeals You have the right to appeal decisions made about your eligibility for programs or certain decisions made about your care. Understanding Terms Understanding Terms You can find some definitions to some more commonly used words throughout Indiana Medicaid. Other Important Social Services Other Important Social Services You can learn about other social services available to you.
You can find answers to frequently asked questions here. Contact Us Contact Us A complete list of phone numbers for coverage and benefit questions. When a drug requires prior authorization it means that the health care provider must ask for approval before the drug can be covered. Drugs may require prior authorization because there is an equally effective low cost alternative, there are safety concerns and/or a potential for inappropriate use. The process for submitting prior authorization requests varies by plan and may be done by phone, fax or electronically. In all cases, providers will need to provide their rationale for covering the drug.
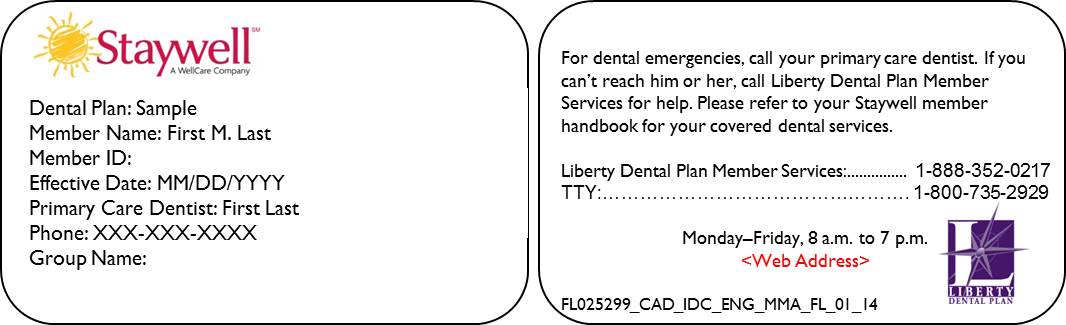
The process for submitting a PA request can be found by contacting the health plan or accessing their web site. Each time you go to your health care provider or pharmacy, take your Medicaid ID and Healthy LA plan ID cards with you. Show them at all medical visits before you receive any service. The health care provider or pharmacy will tell you if they accept your Medicaid benefits. You should also ask your health care provider or pharmacy if the service or prescription is covered by Medicaid before receiving the service or filling a prescription.
Peach State Health Plan is a health plan participating in Georgia Families® . It is a managed care program for Medicaid and PeachCare for Kids® members. We offer our members local healthcare programs and services. Peach State Health Plan helps our members grow healthy and stay healthy. Drugs that are not listed on a health plans formulary may be either non-formulary or covered as a medical benefit.
Non formulary drugs may be covered if the provider or member requests coverage. Hoosier Care Connect Hoosier Care Connect Hoosier Care Connect is a health care program for individuals who are aged 65 years and older, blind, or disabled and who are also not eligible for Medicare. Children who are wards of the State, receiving adoption assistance, foster children and former... Traditional Medicaid Traditional Medicaid Traditional Medicaid is a program created to provide health care coverage to individuals who are not enrolled in managed care. Members normally served in Traditional Medicaid include individuals eligible for both Medicare and Medicaid, individuals who...
A member ID number and group number allow healthcare providers to verify your coverage and file insurance claims for health care services. It also helps UnitedHealthcare advocates answer questions about benefits and claims. Hoosier Healthwise Hoosier Healthwise Hoosier Healthwise is a health care program for children up to age 19 and pregnant women. The program covers medical care like doctor visits, prescription medicine, mental health care, dental care, hospitalizations, and surgeries at little or no cost... Recovery will be made from any real or personal property in the estate of the recipient up to the value of payments made by Medicaid for nursing facility, hospital and drug services. Estate recovery will not apply to recipients who have a surviving spouse, dependent or disabled child.
For more information read the Federal Law on Medicaid Estate Recovery and Mississippi Medicaid Estate Recovery Law. Your member ID number and group number allow healthcare providers to verify your coverage and file claims for health care services. These numbers also help UnitedHealthcare advocates answer questions about your benefits and claims. You might see another list with 2 different percent amounts. The network makes it easier for your health care providers to access your health information. Electronic records also change the way that your PCP and other doctors see your health history.
They can see graphs and charts and easily note trends in your health. It is important to show each health care provider your Medicaid Member Card BEFORE you receive any services. To avoid problems, carry the cards listed below with you each time you seek health care services.
Learn about managed care plans available in your area. Compare different benefits and providers offered by the health plans. Your main doctor is called a primary care provider, or PCP.
Your PCP is listed on your member ID card and in your online account. Call to make an appointment with your PCP as soon as you can. All new Healthy Blue members should see their PCP within 90 days of joining. Getting a checkup now will help your PCP learn about your medical history before any health issues occur.
This website has new tools to help you find and view primary care providers and health plans. A notice of action is a letter sent to both the provider and member which explains why a drug is not covered or is not medically necessary. The notice may also be called an Initial Adverse Determination. The notice explains what rights the member has to appeal the health plan's decision. The notice also gives information on the member's right to a State fair hearing and, if the denial was based on medical necessity, the member's right to an independent external appeal.
Your PCP is listed on your ID card and in your online account. Currently the "lookback" period is 60 months prior to the month you are applying for coverage of nursing home care. Show your ID card every time you visit the doctor, pharmacy, hospital, or any other healthcare provider. Healthcare providers can use your member ID number to review your benefits, and can let you know if you owe any copayments at the time of your visit.
The back or bottom of your health insurance card usually has contact information for the insurance company, such as a phone number, address, and website. This information is important when you need to check your benefits or get other information. For example, you might need to call to check your benefits for a certain treatment, send a letter to your insurance company, or find information on the website. These services may be provided using your Medicaid card or through your managed care plan if you are enrolled in managed care.
You will not have a co-pay if you are in a managed care plan, except for pharmacy services, where a small co-pay will be applied. If you are currently enrolled in a managed care plan that is not offered in the new county, your local department of social services will notify you so that you can choose a new plan. Pregnant women and children can apply at many clinics, hospitals, and provider offices. Call your local department of social services to find out where you can apply. Sunshine Health is a managed care plan with a Florida Medicaid contract. The benefit information provided is a brief summary, not a complete description of benefits.
Limitations, co-payments and restrictions may apply. Benefits, formulary, pharmacy network, premium and/or co-payments/co-insurance may change. For more information contact the Managed Care Plan. We give each person who qualifies for Health First Colorado (Colorado's Medicaid program) an ID Number.
Your and your family or caretaker's Health First Colorado ID Number is sometimes called your State ID Number. Your ID Number is on your Health First Colorado card. It is also on all letters we send you about your benefits. When you go to an appointment with your health care provider, they will ask you for your insurance information. Your health insurance card has important information.
Please make sure you bring it to every appointment. Finally, you might see a dollar amount, such as $10 or $25. This is usually the amount of your co-payment, or "co-pay." A co-pay is a set amount you pay for a certain type of care or medicine. Some health insurance plans do not have co-pays, but many do. If you see several dollar amounts, they might be for different types of care, such as office visits, specialty care, urgent care, and emergency room care.
If you see 2 different amounts, you might have different co-pays for doctors in your insurance company's network and outside the network. To find out if a provider is "in network" contact your insurance company. The "coverage amount" tells you how much of your treatment costs the insurance company will pay.
This information might be on the front of your insurance card. It is usually listed by percent, such as 10 percent, 25 percent, or 50 percent. You might see several percent amounts listed together. For example, if you see 4 different percent amounts, they could be for office visits, specialty care, urgent care, and emergency room care. Each child enrolled in Denali KidCare will receive a Denali KidCare Card.
This card can be used for health care and certain medical related services only for the person named on the card. The coverage period is generally six months and is valid for the period shown on the front of the card. Show your Medicare card to your doctor, hospital, or other health care provider when you get services. NC Medicaid Managed Care health plans are now active. This means that you will now get care through your health plan.
If you have questions about benefits and coverage, call your health plan. You can find the number on your new Medicaid ID card or visit View health plans. Your main doctor is called a primary care provider . Your PCP is listed on your member ID card and on your online account. Getting a checkup now will help your PCP learn about your health history before any health issues occur.
In most health plans, the formulary is developed by a pharmacy and therapeutics committee made up of pharmacists and physicians from various medical specialties. The committee reviews new and existing medications and selects drugs to be in the health plan's formulary based on safety and how well they work. The committee then selects the most cost-effective drugs in each drug class. A drug class is a group of drugs that treat a specific health condition or that work in a certain way. Long-term care supports may be provided either in a facility or in an individual's own home or in the community. The back of your member ID card includes contact information for providers and pharmacists to submit claims.
It also includes the member website and health plan phone number, where you can check benefits, view claims, find a doctor, ask questions and more. If you got a letter stating you've been enrolled in Medicaid or CHIP, you should still be able to get health care services. Show your provider a copy of your eligibility letter. If you're enrolled in a health plan through Medicaid or CHIP, contact the member services phone number on your eligibility letter or the back of your enrollment card.
This information should also be on the websites of your health plan or Medicaid or CHIP agency. ICare specializes in managed care health insurance plans for people at every stage or need in their life. Out-of-network/non- contracted providers are under no obligation to treat UnitedHealthcare plan members, except in emergency situations.
Please call our customer service number or see your Evidence of Coverage for more information, including the cost- sharing that applies to out-of-network services. The Georgia Department of Community Health is one of Georgia's health agencies. DCH's programs provide access to health care services for one in four Georgians.
Learn about Georgia Department of Community Health. The way health plans handle dose changes, for those drugs in which PA was previously obtained and not expired, varies based on each health plans system capabilities. If a new PA is required, submission of the standardized PA form is helpful, as it addresses issues relating to dose titration and dose adjustments.
Managed care covers most of the benefits recipients will use, including all preventive and primary care, inpatient care, and eye care. People in managed care plans use their Medicaid benefit card to get those services that the plan does not cover. Medicare is a federal health insurance program for people age 65 and for certain people with disabilities, regardless of income.
When a person has both Medicare and Medicaid, Medicare pays first and Medicaid pays second. Medicaid provides health coverage to eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. Medicaid is administered by states, according to federal requirements. The program is funded jointly by states and the federal government. The Medicaid program provides health coverage to eligible low-income adults, children, pregnant women, elderly adults and people with disabilities.